What is Monobenzone Powder Used For?
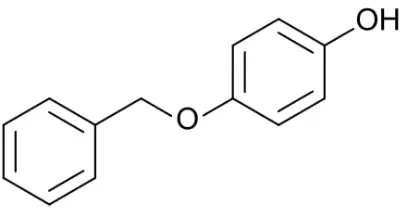
Monobenzone powder, also known as hydroquinone monobenzyl ether or benzyloxy phenol, is a depigmenting agent primarily used in dermatology. This white crystalline powder has gained attention for its ability to permanently lighten skin by selectively destroying melanocytes, the cells responsible for producing melanin. Originally developed as a treatment for vitiligo, Monobenzone powder has evolved to serve various medical and cosmetic purposes. This article explores the applications, mechanisms, and considerations related to Monobenzone powder, providing a comprehensive understanding of this powerful depigmenting agent.
What Are the Medical Applications of Monobenzone Powder?
Treatment for Extensive Vitiligo
Monobenzone powder stands as one of the few FDA-approved treatments for extensive vitiligo when repigmentation therapies fail. When patients have vitiligo affecting more than 50% of their body surface area, Monobenzone powder offers a solution by depigmenting the remaining normal skin to create a uniform appearance. The process involves applying Monobenzone powder formulations consistently over several months. The compound works by permanently destroying melanocytes, resulting in complete depigmentation that matches the vitiligo-affected areas. Medical professionals carefully monitor this treatment as Monobenzone powder creates an irreversible loss of pigmentation, making it a last-resort option when other treatments have proven ineffective. For patients with widespread vitiligo, this approach can significantly improve quality of life by eliminating the patchwork appearance of the skin.
Managing Hyperpigmentation Disorders
Beyond vitiligo treatment, Monobenzone powder has applications in managing certain hyperpigmentation disorders. Under strict medical supervision, dermatologists may prescribe Monobenzone powder for conditions like post-inflammatory hyperpigmentation, melasma, or lentigines when conventional treatments have failed. Unlike temporary lightening agents, Monobenzone powder induces lasting changes by inhibiting tyrosinase—the enzyme crucial for melanin production—and causing melanocyte destruction. The depigmenting effect of Monobenzone powder extends beyond the application area through a phenomenon called "remote depigmentation," where melanocytes distant from the treatment site also lose functionality. This property requires careful consideration before treatment initiation, as medical professionals must weigh the benefits against the permanent nature of the treatment. Patients with localized hyperpigmentation disorders must understand that Monobenzone powder treatment may eventually lead to more widespread lightening.
Therapeutic Uses in Dermatological Research
Monobenzone powder plays a significant role in dermatological research, helping scientists understand melanocyte biology and pigmentation disorders. Researchers utilize Monobenzone powder to study mechanisms of depigmentation, melanocyte destruction, and autoimmune responses in the skin. By examining how Monobenzone powder modifies melanocytes and triggers immune responses against pigment cells, scientists gain insights applicable to various dermatological conditions. The compound has revealed important pathways in melanocyte destruction that may have implications for treating melanoma and other pigment cell disorders. Monobenzone powder research has contributed to understanding cytotoxic T-cell responses to melanocytes, potentially opening new avenues for immunotherapy development. These investigations continue to expand our knowledge of skin biology and may lead to novel therapeutic approaches for pigmentation disorders and skin-related autoimmune conditions.
How Does Monobenzone Powder Work on the Skin?
The Biochemical Mechanism of Depigmentation
Monobenzone powder operates through a complex biochemical mechanism that permanently alters the skin's pigmentation process. When applied topically, Monobenzone powder penetrates the skin and is specifically converted by tyrosinase within melanocytes into reactive quinones. These quinones create oxidative stress and form hapten complexes with melanocyte proteins, essentially marking these cells for destruction by the immune system. Unlike temporary lightening agents that simply inhibit melanin production, Monobenzone powder triggers an autoimmune response against melanocytes. The process involves cytotoxic T-lymphocytes that recognize and attack these modified melanocytes, leading to their permanent destruction. Additionally, Monobenzone powder interferes with melanosome structure and function, disrupting the organelles responsible for melanin synthesis and storage. This multi-faceted approach to melanocyte destruction makes Monobenzone powder particularly effective but also explains its permanent effects on skin pigmentation.
Differences Between Monobenzone Powder and Other Lightening Agents
Monobenzone powder fundamentally differs from other skin lightening agents in both mechanism and permanence. While compounds like hydroquinone, kojic acid, or arbutin temporarily inhibit tyrosinase activity without destroying melanocytes, Monobenzone powder permanently eliminates these pigment-producing cells. Conventional lightening agents allow pigmentation to return once treatment stops, whereas Monobenzone powder's effects persist indefinitely due to the destruction of melanocytes. This distinction makes Monobenzone powder considerably stronger than cosmetic lighteners and explains its restricted medical use. Unlike alpha hydroxy acids or vitamin C derivatives that exfoliate or provide antioxidant effects, Monobenzone powder directly targets the cellular source of pigmentation. The systemic effects of Monobenzone powder also set it apart—it can cause depigmentation in untreated areas through the "confetti-like" or "halo" phenomenon, where melanocytes distant from the application site eventually become targets for immune destruction. These distinctive properties underscore why Monobenzone powder requires medical supervision and isn't suitable for general cosmetic applications.
The Timeline and Permanence of Results
The depigmentation process initiated by Monobenzone powder follows a predictable yet variable timeline. Initial visible results typically emerge after 1-3 months of consistent application, with complete depigmentation potentially requiring 6-12 months or longer depending on individual factors. Once achieved, the results are generally permanent due to the destruction of melanocytes rather than temporary suppression of melanin production. The depigmentation process often progresses unevenly, creating a mottled appearance before achieving uniform lightening. Even after treatment cessation, the depigmenting effect may continue to develop in previously untreated areas due to the autoimmune response triggered by Monobenzone powder. This extended timeline requires patient commitment and consistent follow-up with healthcare providers. The permanence of Monobenzone powder treatment necessitates lifelong sun protection, as the treated skin loses its natural defense against UV radiation. Without melanin's protective function, the skin becomes highly susceptible to UV damage, requiring diligent use of broad-spectrum sunscreens, protective clothing, and sun avoidance strategies.

Who Should Consider Using Monobenzone Powder?
Ideal Candidates for Monobenzone Treatment
The ideal candidates for Monobenzone powder treatment are individuals with extensive vitiligo affecting more than 50% of their body surface area who have not responded to conventional repigmentation therapies. These patients often experience significant psychological distress from the patchy appearance of their skin and seek uniform coloration. Candidates should demonstrate stable disease without active spreading of depigmented areas for at least six months before considering Monobenzone powder treatment. Patients must possess the commitment to follow through with the lengthy treatment process and understand the permanence of the results. Psychological readiness is equally important—candidates should comprehend and accept the irreversible nature of depigmentation and its implications for lifelong sun protection. Medical screening ensures candidates have no contraindications such as pregnancy, lactation, or certain autoimmune conditions that might be exacerbated by Monobenzone powder. The decision to pursue Monobenzone powder treatment should follow thorough discussions with dermatologists specializing in pigmentation disorders who can provide realistic expectations about outcomes.
Precautions and Contraindications
Several important precautions and contraindications exist for Monobenzone powder use. Pregnant or breastfeeding women should strictly avoid Monobenzone powder due to potential systemic absorption and unknown effects on fetal development or nursing infants. Individuals with a history of skin cancer face increased risk as Monobenzone powder removes melanin's protective benefits against UV radiation. Those with autoimmune disorders require careful evaluation before Monobenzone powder treatment, as the therapy can potentially trigger or exacerbate certain autoimmune conditions through its immunological effects. Patients with known sensitivity to hydroquinone derivatives or phenolic compounds should avoid Monobenzone powder due to potential allergic reactions. Children generally should not receive Monobenzone powder treatment except in exceptional cases with extensive vitiligo, requiring thorough risk-benefit analysis. Individuals unable to commit to rigorous, lifelong sun protection measures are poor candidates for Monobenzone powder therapy. Those with unrealistic expectations about treatment timeline or cosmetic outcomes should reconsider, as the process requires patience and acceptance of potential unevenness during the depigmentation phase.
Professional Application and Monitoring
Professional guidance is essential throughout the Monobenzone powder treatment journey. Dermatologists specialized in pigmentation disorders conduct comprehensive assessments before prescribing, including medical history review, physical examination, and possibly skin biopsies to confirm diagnoses. Treatment typically begins under close supervision with regular follow-up appointments to monitor progress and potential adverse effects. Healthcare providers establish individualized treatment protocols specifying concentration (typically 20-40% Monobenzone powder in cream formulations), application frequency, and expected timeline. During follow-up visits, documentation of depigmentation progress through standardized photography helps track treatment effectiveness. Medical professionals monitor for side effects like contact dermatitis, irritation, or unexpected systemic effects and adjust treatment accordingly. They provide guidance on complementary measures such as sun protection strategies, cosmetic camouflage during the transition period, and psychological support resources. The monitoring process extends beyond the active treatment phase, with long-term follow-up recommended to assess maintenance of results and screen for potential complications like photodamage or skin malignancies. This professional oversight ensures Monobenzone powder is used safely and effectively while minimizing risks associated with this powerful depigmenting agent.
Conclusion
Monobenzone powder represents a specialized depigmentation treatment primarily for extensive vitiligo when other options have failed. Its permanent action through melanocyte destruction distinguishes it from temporary lightening agents. While effective for specific medical conditions under professional supervision, its irreversible nature demands careful patient selection and lifelong sun protection. Understanding its mechanisms, applications, and limitations is essential for appropriate use in dermatological practice.
Shaanxi Yuantai Biological Technology Co., Ltd. (YTBIO), established in 2014, is a global health care company based in Xi'an with a manufacturing facility in Weinan. We specialize in health food ingredients (such as Herbal Extracts, Magnesium Threonate, and Creatine Monhydrate) and cosmetic ingredients (including Sponge Spicule, Retinol, Glutathione, and Arbutin). We work with partners in Europe, America, Southeast Asia, and Korea. With a warehouse in Rotterdam for EU distribution and plans for U.S. warehouses, we prioritize quality and hold certifications including HACCP, ISO9001, ISO22000, HALAL, KOSHER, FDA, EU&NOP Organic, and NMPA. We also assist Korean clients with KFDA registration. Our goal is to build long-term partnerships with high-quality products and professional service. For inquiries, contact us at sales@sxytorganic.com or +86-029-86478251 / +86-029-86119593.
References
1. Nordlund JJ, Grimes PE, Ortonne JP. The safety of hydroquinone monobenzyl ether (Monobenzone) and its efficacy in clinical treatments of vitiligo. Journal of the American Academy of Dermatology. 2006;54(2):236-245.
2. Mysore V, Shashikiran BM. Targeted phototherapy in vitiligo and emerging treatment options. Indian Journal of Dermatology, Venereology and Leprology. 2016;82(1):1-8.
3. Harris JE. Chemical-induced vitiligo: Understanding mechanistic basis for treatment design. Experimental Dermatology. 2018;27(5):544-551.
4. Teulings HE, Overkamp M, Ceylan E, et al. Decreased risk of melanoma and nonmelanoma skin cancer in patients with vitiligo: a survey among 1307 patients and their partners. British Journal of Dermatology. 2013;168(1):162-171.
5. Van den Boorn JG, Konijnenberg D, Dellemijn TA, et al. Autoimmune destruction of skin melanocytes by perilesional T cells from vitiligo patients. Journal of Investigative Dermatology. 2009;129(9):2220-2232.
6. Grimes PE, Nashawati R. Depigmentation Therapies for Vitiligo. Dermatologic Clinics. 2017;35(2):219-227.
_1737093401309.png)
